Xenotransplantation: Exploring Benefits, Risks, and Future Directions
What is Xenotransplantation
Definition and explanation of xenotransplantation
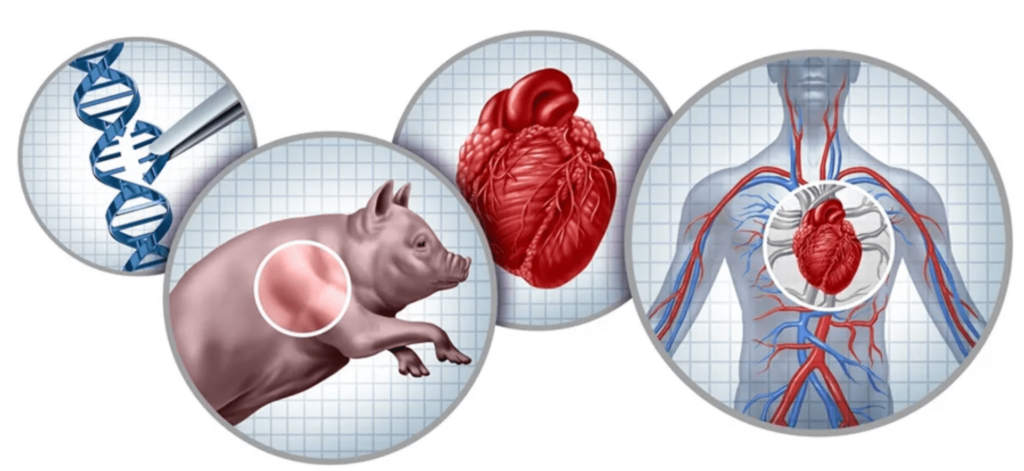
Xenotransplantation is the transplantation of living cells, tissues, or organs from one species to another.
It involves using non-human cells(pig cells), tissues, or an animal organ, like genetically engineered pig kidneys, to treat human medical conditions.
Xenotransplantation is an artificial method of creating an animal-human chimera, where a human has a subset of animal cells.
Brief history of xenotransplantation
- In 1963, doctors at Tulane University attempted chimpanzee-to-human renal transplantations, but the procedure was unsuccessful.
- The first successful xenotransplantation was performed in 1984, when a baboon heart was transplanted into an infant girl, but she died due to a humoral-based graft rejection.
Current state of xenotransplantation research
- Xenotransplantation is an experimental treatment only allowed in extremely rare and serious cases.
- The FDA has not yet allowed clinical trials to begin.
- The goal is to find alternative sources for organs to save lives.
Xenotransplantation in Iran
Xenotransplantation research in Iran is gaining momentum, with local scientists exploring the potential of using animal organs to address the country’s organ shortage. Iranian researchers are focusing on the use of genetically modified pig organs, as pigs are considered a viable donor species due to their physiological similarities to humans. The ethical and religious implications of using pig organs are also being carefully considered, ensuring that any advancements align with cultural and religious values. As Iran continues to advance in the field of medical research, xenotransplantation holds promise as a future solution to the growing demand for organ transplants in the region.
Benefits of Xenotransplantation
Addressing organ shortage through organ transplantation
- Xenotransplantation may provide a plentiful source of organs, in lieu of human organs, for transplantation.
- The most important reason for interest in xenotransplantation today is to provide a plentiful source of organs for transplantation.
- Organ transplantation is mainly undertaken to treat severe failure of the kidneys, liver, heart, and lungs.
Potential for improved graft survival
Xenotransplantation has the potential to address the shortage of available organs. Immune responses play a crucial role in graft survival, influencing the success of xenotransplants.
Many studies have been conducted in animals, transferring pig organs into baboons. These studies have shown that transplanting organs across animal species is possible. Natural killer cells are significant in xenotransplantation, contributing to cytotoxicity against xenogenic cells and affecting graft outcomes. The use of genetically modified pig organs has further improved graft survival by minimizing immunogenic reactions and reducing the risk of organ rejection.
Reduced risk of rejection
- The use of genetically engineered pigs can reduce the risk of rejection.
- Genetically engineered pigs can be bred to express human genes and reduce the risk of rejection.
- The introduction of human genes in porcine donors can help mitigate the immune response.
Risks and Challenges
Immunological barriers
Xenotransplantation involves the transplantation of organs or tissues from one species to another.
Human organs are in short supply, making xenotransplantation a potential solution.
Endothelial cells play a crucial role in the immune response and are activated during xenotransplantation. Acute vascular rejection is a type of rejection that occurs in xenotransplantation, characterized by an inflammatory response involving antibodies, macrophages, and platelets. Overcoming acute vascular rejection requires complex strategies, including various immunosuppressive methods to manage immune responses and facilitate successful graft acceptance and organ transplantation. It is associated with endothelial activation and the coagulation process, typically emerging within a few days following transplantation if hyperacute rejection does not occur.
Coagulation and thrombosis
Organ xenografts are plagued by coagulation and thrombosis.
Porcine von Willebrand factor and loss of porcine tissue factor inhibitor contribute to coagulation disorders.
Genetic modification of the organ-source pig to express human complement regulatory proteins and anticoagulant genes may overcome coagulation dysregulation. Endothelial cell activation plays a crucial role in these coagulation disorders, as it can lead to procoagulant and proinflammatory states that affect graft survival.
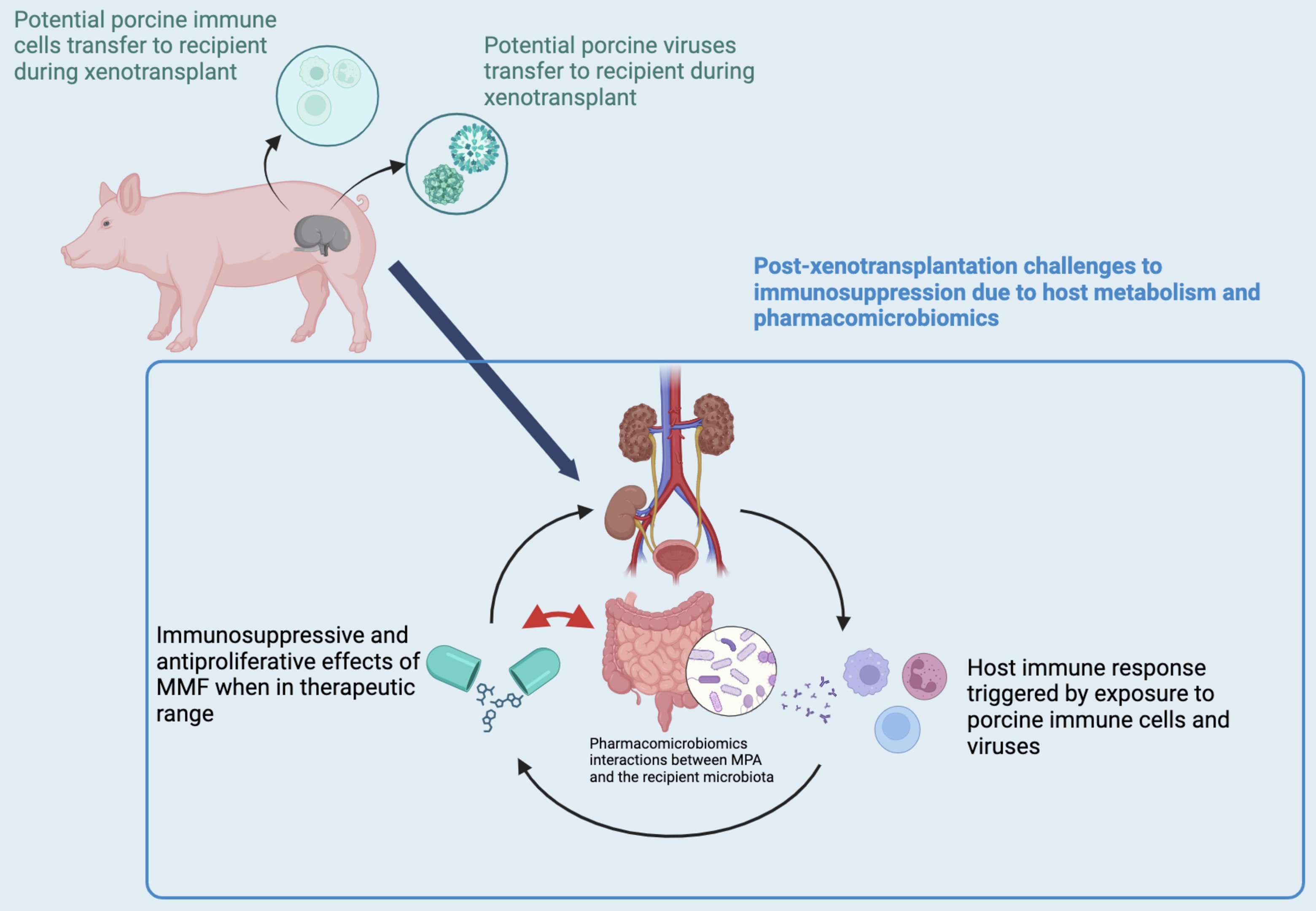
Infectious disease transmission
The potential transfer of infectious organisms from porcine organs to the recipient may imperil the health of the community.
Cell fusion may facilitate transmission of viruses and contribute to emergence of novel viruses.
Xenosis refers to the transmission of infections by the organ transplantation of xenogeneic tissues or organs. The use of porcine cells in xenotransplantation poses risks, including the potential transfer of porcine endogenous retroviruses (PERV) and the immunological barriers that may arise due to the presence of porcine cells within a human recipient.
Porcine endogenous retroviruses (PERVs)
- Porcine endogenous retroviruses (PERVs) are a type of virus that can infect human cells.
- PERVs are a concern in xenotransplantation because they can potentially infect human cells and cause disease.
- The use of genetically engineered pigs can reduce the risk of PERV transmission.
Choosing the Donor Species
Overview of potential donor species
Nonhuman primates, such as chimpanzees and baboons, were first considered as potential organ sources for xenotransplantation to humans.
Pigs are currently thought to be the best candidates for organ donation due to their increased phylogenetic distance from humans and the decreased risk of cross-species disease transmission. The use of animal organs, particularly from pigs, is being extensively researched and tested in clinical trials, addressing challenges like immune rejection and zoonosis.
Immunological considerations
- The ideal donor species for xenotransplantation is a nonhuman primate, but this is not feasible due to ethical concerns.
- Pigs are a more suitable donor species due to their availability, reproductive characteristics, and genetic engineering capabilities.
Coagulation dysregulation as a barrier
Coagulation dysregulation stands as a significant barrier in the field of xenotransplantation. This issue arises primarily due to the activation of endothelial cells (ECs) and the subsequent loss of anticoagulant regulators on their surface, which leads to a procoagulant phenotype. When a pig organ is transplanted into a primate, the immune response against the graft, coupled with molecular incompatibilities between the species, can trigger this coagulation dysregulation.
Genetically engineered pigs that express human complement regulatory proteins (hCRPs) and alpha 1,3 GT-KO pigs have made strides in overcoming hyperacute rejection. However, acute humoral xenograft rejection (AHXR) remains a formidable challenge. AHXR is characterized by microvascular thrombosis and consumptive coagulopathy, often resulting from the binding of antibodies to the graft. This binding activates the complement system and the coagulation cascade, leading to severe complications.
To improve the safety and efficacy of xenotransplantation, ongoing research is focused on developing new treatments and technologies. These advancements aim to mitigate the effects of coagulation dysregulation and enhance the overall success of xenotransplantation procedures.
Genetically Engineered Pigs
Introduction to genetic engineering in xenotransplantation
Genetic engineering is used to modify the donor species to reduce the risk of rejection and improve graft survival. The use of soluble complement receptor type 1 (sCR1) as a therapeutic agent has shown promise in preventing hyperacute rejection during xenotransplantation. The use of genetically engineered pigs can reduce the risk of rejection and improve graft survival.

Incorporating human genes in porcine donors
Incorporating human genes into porcine donors represents a promising strategy to overcome the immunological barriers associated with xenotransplantation. Through genetic engineering, human genes can be introduced into porcine donors to reduce the risk of rejection and improve the survival rates of xenografts.
Key human genes that have been incorporated into porcine donors include those involved in the regulation of the complement system, such as CD46, CD55, and CD59. These genes play a crucial role in preventing the activation of the complement system, thereby reducing the risk of rejection. Genetic testing can also help with the success rate. Additionally, genes involved in the regulation of the coagulation cascade, such as TFPI and CD39, have been introduced to prevent the activation of the coagulation cascade and reduce the risk of thrombosis.
Preclinical studies have shown promising results with genetically engineered porcine donors expressing these human genes. This approach offers a new avenue for overcoming the immunological barriers to xenotransplantation, potentially paving the way for more successful and widespread use of xenotransplantation in the future.
Use of human cells in xenotransplantation
- Human cells can be used in xenotransplantation to reduce the risk of rejection and improve graft survival.
- The use of human cells in xenotransplantation is still in its infancy and requires further research.
Safety and Efficacy
Mitigating safety concerns
The use of genetically engineered pigs can reduce the risk of rejection and improve graft survival.
The introduction of human genes in porcine donors can help mitigate the immune response.
The use of human cells in xenotransplantation can reduce the risk of rejection and improve graft survival. However, there are ongoing concerns about the potential transfer of porcine endogenous retrovirus (PERV) during pig-to-human organ transplants, as PERV can infect human cells in culture and pose zoonotic risks to human health.
Overcoming Challenges
Future Directions
Humanized porcine donors
- The use of humanized porcine donors can reduce the risk of rejection and improve graft survival.
- Humanized porcine donors can be bred to express human genes and reduce the risk of rejection.
Emerging technologies and innovations
- Emerging technologies and innovations, such as gene editing and stem cell therapy, can improve the safety and efficacy of xenotransplantation.
- The use of emerging technologies and innovations can reduce the risk of rejection and improve graft survival.
Ethical Considerations
Beneficence and risk-to-benefit analysis
- The potential benefits of xenotransplantation must be weighed against the potential risks.
- The use of xenotransplantation must be justified by the potential benefits and the lack of alternative treatments.
Autonomy and informed consent
- Patients must be fully informed of the potential risks and benefits of xenotransplantation.
- Patients must provide informed consent before undergoing xenotransplantation.
Xenotourism and animal-related ethical issues
- Xenotourism, or the practice of traveling to another country for xenotransplantation, raises ethical concerns.
- The use of animals in xenotransplantation raises ethical concerns, including the treatment of animals and the potential for exploitation.
Regulatory Framework
Current regulations and guidelines
- The FDA regulates xenotransplantation products under section 351 of the US Public Health Service Act and the Federal Food, Drug, and Cosmetic Act.
- The International Xenotransplantation Association (IXA) and the World Health Organization (WHO) are also involved in regulations and guidelines.
Future directions for regulatory frameworks
- Regulatory frameworks must be developed to address the unique challenges of xenotransplantation.
- Regulatory frameworks must balance the need for safety and efficacy with the need for innovation and progress.
Public Perception and Awareness
Understanding public attitudes towards xenotransplantation
- Public attitudes towards xenotransplantation are complex and multifaceted.
- Public awareness and education are essential for promoting understanding and acceptance of xenotransplantation.
Education and awareness efforts
- Education and awareness efforts must be directed towards the general public, healthcare professionals, and policymakers.
- Education and awareness efforts must address the potential benefits and risks of xenotransplantation.
Conclusion
Summary of key points
- Xenotransplantation is a complex and multifaceted field that raises many ethical, regulatory, and scientific challenges.
- The use of genetically engineered pigs and human cells can reduce the risk of rejection and improve graft survival.
- Emerging technologies and innovations can improve the safety and efficacy of xenotransplantation
