Dialysis for Kidneys Explained:Types, Benefits, and Thriving with Treatment
Chronic Kidney Disease, Kidney Failure and Dialysis for kidneys
Kidney failure also known as end-stage renal disease (ESRD) happens when kidneys lose the ability to filter waste and excess fluid from the blood. Chronic kidney disease has long term effects on patients’ overall health and treatment includes various options and strategies especially for those who may not want to do dialysis. Dialysis is a treatment that filters waste products from the blood when kidneys are not healthy enough to do so.
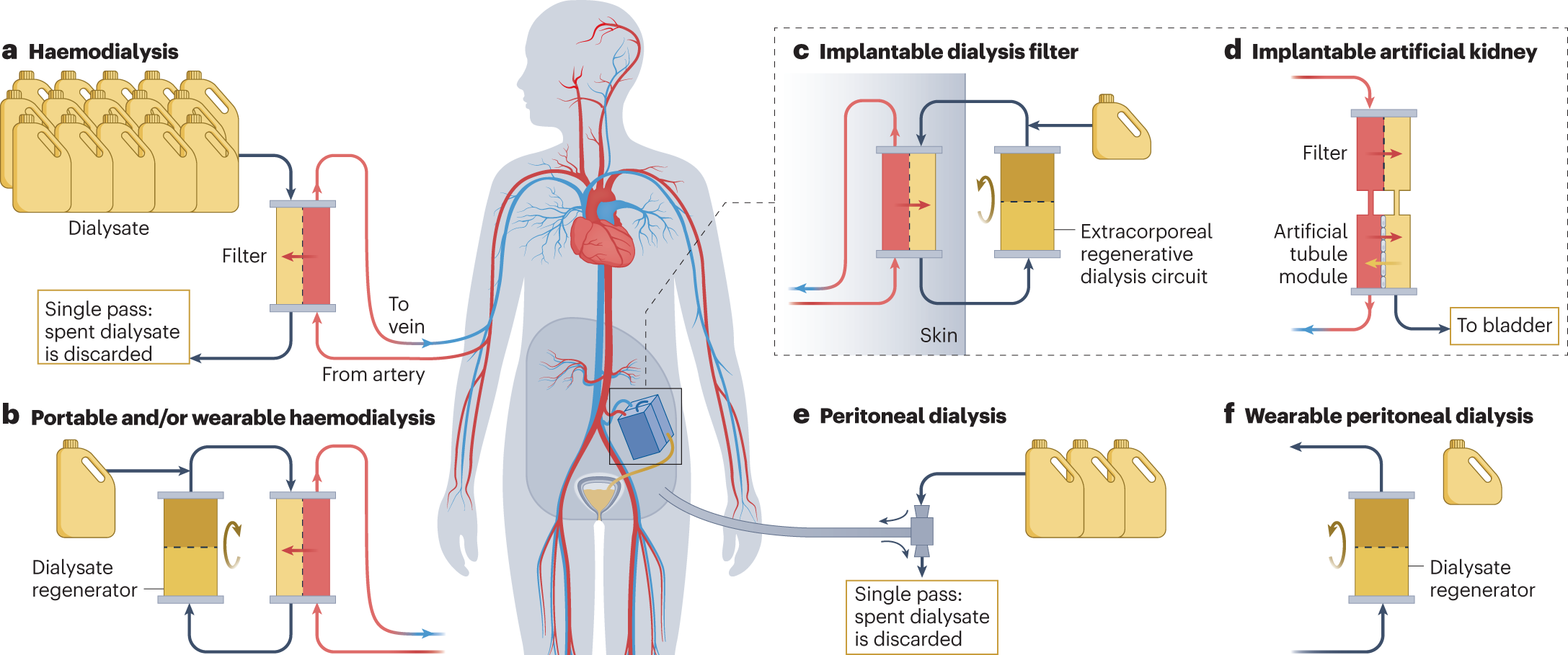
There are two types of dialysis: hemodialysis and peritoneal dialysis.
Dialysis helps manage kidney disease and improves quality of life.
What is Dialysis?
Dialysis is a medical treatment that takes over the functions of the kidneys when they can no longer function properly due to end-stage renal disease (ESRD) or acute kidney injury. This life-saving procedure removes waste products and excess fluids from the blood that the kidneys would normally handle. There are two main types of dialysis: hemodialysis and peritoneal dialysis. Each type uses different methods to achieve the same goal of maintaining the body’s balance of fluids and electrolytes so patients can still live healthy despite severe kidney function impairment. In addition to dialysis, a renal transplant is another treatment option for individuals with kidney failure. A renal transplant involves replacing a failing kidney with a healthy kidney from a donor, offering the potential for improved quality of life and kidney function without the need for ongoing dialysis treatments.
Types of Dialysis
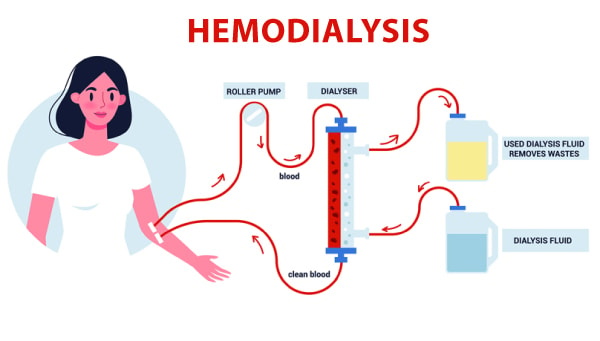
Hemodialysis
Hemodialysis uses a machine to filter blood outside the body.
The process takes 3-5 hours and is done 3 times a week at a dialysis center or hospital. Blood vessels such as arteries and veins are surgically accessed to facilitate high blood flow during hemodialysis.
Hemodialysis can control blood pressure and balance important minerals in the blood. But low blood pressure is a side effect some may experience during or after hemodialysis with symptoms like nausea, dizziness or faintness.
Hemodialysis can be done at home with a dialysis machine.
Peritoneal Dialysis
- Peritoneal dialysis uses the lining of the abdominal cavity to filter blood.
- A dialysis solution is used to clean the blood and remove waste products.
- Peritoneal dialysis can be done at home with a catheter and dialysis solution.* Continuous ambulatory peritoneal dialysis (CAPD) is a type of peritoneal dialysis that uses manual exchange of dialysis solution.
Hemodialysis vs Peritoneal Dialysis
When it comes to dialysis treatments patients have two main options: hemodialysis and peritoneal dialysis. Hemodialysis uses a dialysis machine to filter the blood outside the body. This is done in a dialysis center or can be done at home with the right equipment and training. Peritoneal dialysis uses the lining of the abdominal cavity (peritoneum) to filter the blood internally. This is done at home and offers more flexibility and independence. Each type of dialysis has its own advantages and disadvantages and the choice between them depends on individual patient needs, lifestyle and medical advice.
Preparing for Dialysis
Preparation for dialysis means understanding the treatment options and making lifestyle changes. Testing kidney function through medical tests like eGFR is crucial to determine if dialysis is needed.
Patients with kidney disease should protect their blood vessels by avoiding needle sticks and IV lines.
Vascular access surgery may be necessary to create a lifeline for dialysis.
Patients should also follow a healthy diet and lifestyle to manage kidney disease.
Pre-Dialysis Steps
Before starting dialysis treatment patients undergo several preparatory steps to make the process as smooth and comfortable as possible. One of the first steps is creating a vascular access such as an arteriovenous fistula or graft which allows for easy and efficient access to the bloodstream for hemodialysis. For those who will be doing peritoneal dialysis a catheter will be surgically inserted into the peritoneal cavity. Patients will also undergo a series of blood tests to help their healthcare team determine the best dialysis treatment plan. Meeting with a dietitian is also important to discuss dietary restrictions and recommendations specific to their condition. Education and training sessions are provided to help patients understand and manage their dialysis treatment.
The Dialysis Process
- The dialysis process filters waste products from the blood using a dialysis machine or peritoneal dialysis solution.
- Each dialysis session takes about 4 hours and is done on a set schedule usually 3 times a week.
- Peritoneal dialysis can be done at home with a catheter and dialysis solution.* Patients should follow their healthcare provider’s instructions for medication and fluid intake.
How Dialysis Works
Dialysis works by using a semipermeable membrane to filter waste products and excess fluids from the blood, mimicking the natural function of healthy kidneys. In hemodialysis, the patient’s blood is pumped through a dialyzer, which contains the semipermeable membrane. This dialyzer acts as an artificial kidney, filtering out toxins and excess fluids before returning the cleansed blood to the body. Peritoneal dialysis involves infusing a special fluid called dialysate into the peritoneal cavity. The peritoneal membrane acts as the filter, allowing waste products and excess fluids to pass from the blood into the dialysate, which is then drained from the body. Both methods remove harmful substances and maintain the body’s fluid and electrolyte balance.
Additionally, for those considering a kidney transplant as an alternative to dialysis, it’s important to understand the associated costs. Kidney transplant cost can vary significantly based on factors like the healthcare facility, geographic location, and the patient’s specific medical needs. Understanding these costs is crucial for planning and making informed decisions about treatment options.
Life on Dialysis
Life on dialysis means making lifestyle changes to accommodate treatment sessions. Patients should follow a healthy diet and lifestyle to manage kidney disease. Patients should also monitor their blood pressure and weight to get the best possible results from dialysis. Muscle cramps can be a side effect of hemodialysis treatments especially due to sudden changes in the body’s water and chemical balance during these treatments. Stay hydrated is important but patients should avoid excessive fluid intake between dialysis treatments.
Diet and Nutrition for Dialysis Patients
A well planned diet is essential for dialysis patients to maintain overall health and manage kidney disease. A kidney dietitian can help create a personalized meal plan that takes into account the patient’s nutritional needs, lifestyle and food preferences.
Key Principles of a Dialysis Diet
- Fluid Management: Limiting fluid intake is crucial to prevent fluid buildup in the body which can lead to complications such as swelling and high blood pressure.
- Electrolyte Balance: Managing electrolyte levels such as potassium, sodium and phosphorus is vital to prevent complications like heart problems and bone disease.
- Protein Intake: Consuming adequate protein helps maintain muscle mass and overall health which is especially important for dialysis patients.
- Sodium and Phosphorus Restriction: Limiting sodium and phosphorus intake helps prevent fluid buildup and bone disease which are common concerns for dialysis patients.
- Calcium and Vitamin D Management: Managing calcium and vitamin D levels is important to prevent bone disease and overall health.
Foods to Include and Avoid
- Include: Fresh fruits, vegetables, whole grains, lean proteins and low-fat dairy products are good for dialysis patients.
- Avoid: Processed and high-sodium foods, sugary drinks and foods high in phosphorus and potassium should be limited to prevent complications.
Supplements and Vitamins
- Vitamin D: For bone health and immune function.
- Calcium: For bone health and muscle function.
- Iron: For healthy red blood cells.
- B Vitamins: For energy production and nerve function.
Tips for Healthy Eating
- Eat Small, Frequent Meals: To manage hunger and prevent overeating.
- Choose Low-Sodium Options: When cooking and eating out.
- Read Food Labels: To make informed choices about sodium, phosphorus and potassium content.
- Stay Hydrated: Drink water and other low-sodium fluids to prevent dehydration.
By following a well planned diet and staying hydrated dialysis patients can manage their kidney disease, prevent complications and live a good quality of life.
Psychological and Emotional Support
Living with kidney disease and undergoing dialysis can be emotionally challenging. Patients may experience anxiety, depression and stress which can impact their overall well-being and treatment outcomes.
Importance of Emotional Support
- Coping with Diagnosis: Receiving a diagnosis of kidney disease can be overwhelming and emotional support can help patients cope with their emotions.
- Managing Treatment-Related Stress: Dialysis treatments can be time consuming and stressful and emotional support can help patients manage their stress levels.
- Maintaining Relationships: Kidney disease can impact relationships with family and friends and emotional support can help patients maintain these relationships.
Types of Emotional Support
- Counseling: One-on-one counseling with a mental health professional can help patients manage their emotions and develop coping strategies.
- Support Groups: Joining a support group can provide patients with a sense of community and connection with others who are experiencing similar challenges.
- Family Therapy: Family therapy can help patients and their loved ones communicate effectively and manage the emotional impact of kidney disease.
Tips for Managing Emotional Well-being
- Stay Connected: Maintain relationships with family and friends to prevent feelings of isolation.
- Practice Self-Care: Engage in activities that bring joy and relaxation, such as reading, exercise or meditation.
- Seek Professional Help: Don’t hesitate to seek counseling or therapy if emotional challenges become overwhelming.
By acknowledging the emotional impact of kidney disease and seeking support patients can manage their emotional well-being and overall quality of life.
Managing Discomfort and Side Effects
Dialysis is a life saving treatment but it can come with some discomfort and side effects such as low blood pressure, muscle cramps and nausea. To manage these issues and improve their quality of life patients can take several proactive steps. Following a healthy diet and lifestyle is essential as is staying hydrated and managing fluid intake to prevent complications. Taking medications as prescribed by their healthcare team can help mitigate side effects. Regular exercise and physical activity can also improve overall well-being and reduce discomfort. Practicing stress-reducing techniques like meditation or deep breathing can help manage the emotional and physical stress associated with dialysis. By adopting these strategies patients can manage their symptoms and live a better life on dialysis.
Life Expectancy and Kidney Transplant Options
- Life expectancy on dialysis varies depending on medical conditions, treatment adherence and other factors.
- Average life expectancy on dialysis is 5-10 years but many patients have lived well on dialysis for 20-30 years.
- Kidney transplantation is a treatment option for patients with end-stage renal disease.
- Patients should discuss transplant options with their healthcare provider.
Global Dialysis Access and Clinical Trials
- Dialysis access varies globally with some countries having limited access to dialysis centers.
- Clinical trials are ongoing to improve dialysis treatment and patient outcomes.
- Patients can participate in clinical trials to contribute to the development of new treatments.
- Patients should discuss clinical trial options with their healthcare provider.
Technological Advances in Dialysis
Technology has advanced dialysis treatments making them more efficient, effective and comfortable for patients.

Recent Advances
- Home Dialysis Machines: Portable and user-friendly machines have made home dialysis more accessible and convenient, patients can receive treatment in the comfort of their own homes.
- Automated Peritoneal Dialysis: Automated systems have simplified the peritoneal dialysis process reducing the risk of infection and improving treatment outcomes.### Dialysis Software
Software has improved treatment monitoring and data analysis, enabling healthcare providers to make better decisions.
Future
- Wearable Dialysis Devices: Devices that can do dialysis on-the-go are being developed, giving patients more freedom.
- Artificial Kidney: Researchers are working on an artificial kidney that can replace dialysis, a cure for kidney disease.
- Personalized Medicine: Genomics and precision medicine are enabling healthcare providers to tailor dialysis to individual patients.
Benefits
- Better Outcomes: Technology has improved outcomes, reducing complications and patient mortality.
- Patient Comfort: New technology has made dialysis more comfortable and convenient, better quality of life.
- Patient Engagement: Technology has empowered patients to take more control of their care, better adherence and outcomes.
By embracing technology patients and healthcare providers can work together to improve dialysis and get better results.
Cost and Insurance
Dialysis is expensive and understanding the cost and insurance is key for patients and their families.
Costs
- Treatment Costs: Dialysis treatment can cost thousands of dollars a month depending on the type and frequency of treatment.
- Medication Costs: Patients may need to take medication for their kidney disease which adds to the overall cost of care.
- Travel and Accommodation Costs: Patients may need to travel to dialysis centers or hospitals for treatment, additional costs.
Insurance
- Medicare: Medicare covers dialysis for patients with ESRD.
- Medicaid: Medicaid may cover dialysis for patients who meet income and eligibility requirements.
- Private Insurance: Private insurance may cover dialysis but coverage and cost varies.
Tips to Manage Costs
- Understand Your Insurance: Patients should understand their insurance coverage and out of pocket costs to plan.
- Seek Financial Assistance: Patients may be eligible for financial assistance programs or grants to help with treatment costs.
- Budget and Plan: Patients should budget and plan for treatment costs, travel and accommodation. By understanding the costs and insurance options for dialysis patients and their families can manage their expenses and focus on their health and well-being.
Patient Stories
Living with kidney disease and dialysis can be tough and emotional. Hearing from other patients can be comforting, supportive and inspiring.
- John’s Story: John was diagnosed with kidney disease at 30 and started dialysis shortly after. He talks about his dialysis experience and how it’s affected his life.
- Sarah’s Story: Sarah was diagnosed with kidney disease during pregnancy and did dialysis while pregnant. She talks about her dialysis experience and how it’s affected her family.
- Mark’s Story: Mark was diagnosed with kidney disease at 50 and started dialysis. He talks about his dialysis experience and how it’s affected his relationships and daily life.
Common Themes
- Emotional Challenges: Patients often face emotional challenges like anxiety and depression when living with kidney disease and dialysis.
- Treatment Adherence: Patients often struggle with treatment adherence, including following dietary restrictions and attending dialysis sessions.
- Support Systems: Patients often rely on support systems like family and friends to cope with emotional and physical challenges of kidney disease and dialysis.
Tips to Cope
- Stay Positive: Patients should focus on staying positive and finding ways to manage their emotions.
- Seek Support: Patients should seek support from family, friends and support groups to cope with emotional challenges of kidney disease and dialysis.
- Self-Care: Patients should prioritize self-care, exercise, meditation and relaxation techniques to manage stress and overall well-being.
By sharing their stories patients can comfort, support and inspire others living with kidney disease and dialysis.
